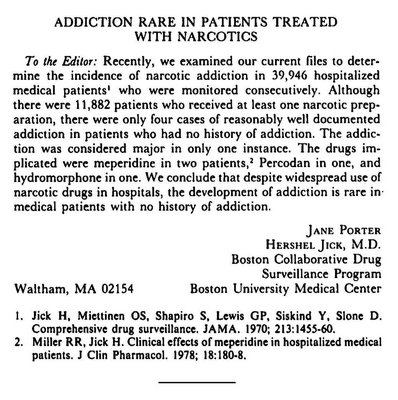
The brief letter published in the New England Journal of Medicine in 1980 that was cited more than 600 times by studies challenging that opioids were dangerously addictive. Some say the letter helped spark the current opioid crisis.
An example of the laminated printout of cartoon faces, rating pain from a wide grin to a deep frown.
Ann Favilla of East Quogue at the St. Rosalie's Community Center Auditorium in Hampton Bays on Tuesday morning to grieve her taxes. DANA SHAW
Dr. Shawn Cannon, an internist in Amagansett who specializes in the treatment of opioid addiction. DANA SHAW
The gardens at the home on Ocean Road in Bridgehampton. DANA SHAW
A squatter was living in a Hampton
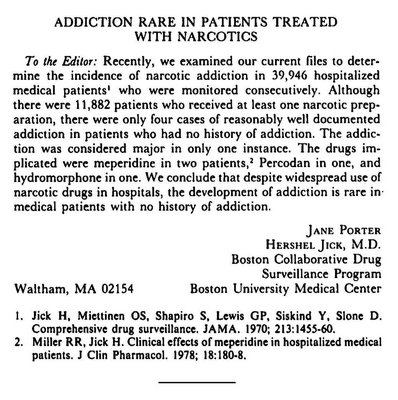
The brief letter published in the New England Journal of Medicine in 1980 that was cited more than 600 times by studies challenging that opioids were dangerously addictive. Some say the letter helped spark the current opioid crisis.
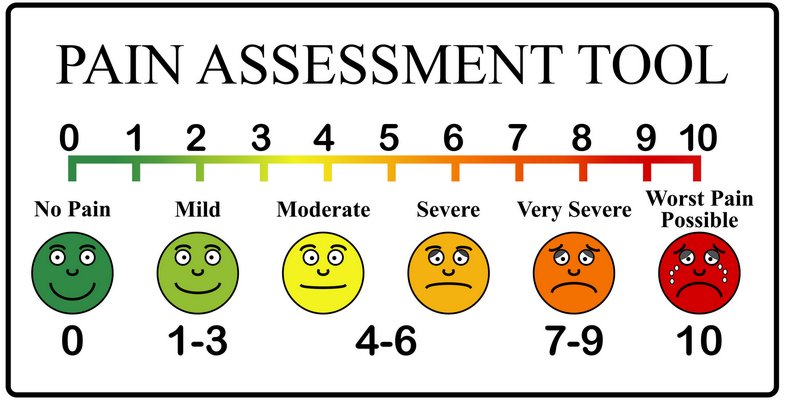
An example of the laminated printout of cartoon faces, rating pain from a wide grin to a deep frown.

Ann Favilla of East Quogue at the St. Rosalie's Community Center Auditorium in Hampton Bays on Tuesday morning to grieve her taxes. DANA SHAW

Dr. Shawn Cannon, an internist in Amagansett who specializes in the treatment of opioid addiction. DANA SHAW


The gardens at the home on Ocean Road in Bridgehampton. DANA SHAW

A squatter was living in a Hampton
We're happy you are enjoying our content. You've read 4 of your 7 free articles this month. Please log in or create an account to continue reading.
Login / Create AccountWe're happy you are enjoying our content. Please subscribe to continue reading.
Subscribe Already a Subscriber


